Osteoporosis: Causes, Symptoms and Treatment in Delhi
Overview
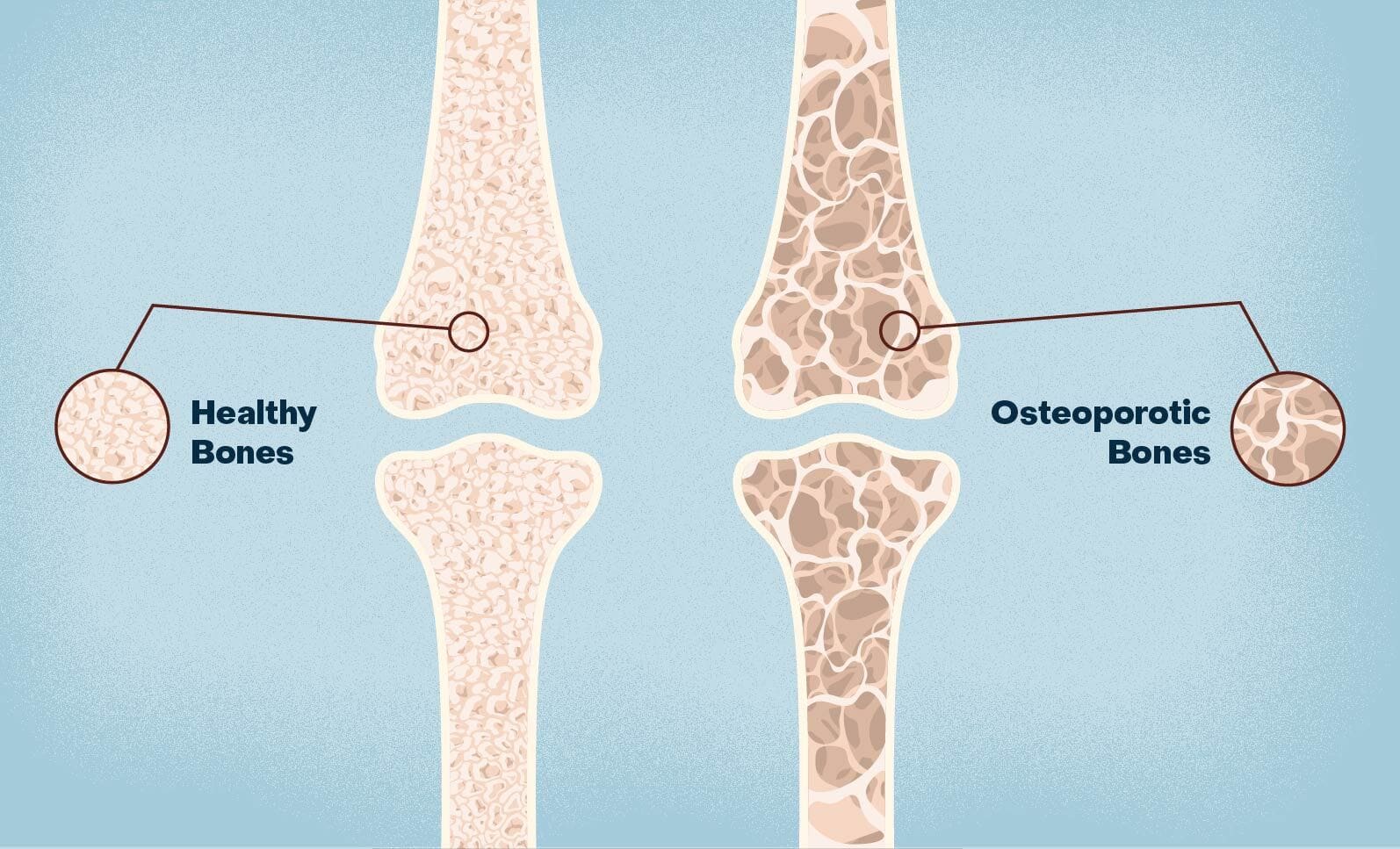
Osteoporosis is a chronic condition where bones become brittle, fragile, and susceptible to fractures due to a decrease in bone density and mass. This bone deterioration happens gradually, often without symptoms until a fracture occurs. Osteoporosis primarily affects postmenopausal women, older adults, and individuals with specific risk factors, such as genetic predisposition, lifestyle choices, and certain medical conditions or medications.
Causes of Osteoporosis
- Aging: Bone density peaks around age 30 and gradually decreases thereafter. With aging, bone regeneration slows down, leading to bone loss.
- Hormonal Changes: Estrogen plays a significant role in bone density. In women, estrogen levels drop after menopause, increasing the risk of osteoporosis. Men also experience bone density loss with age, often linked to lower testosterone levels.
- Nutritional Deficiencies: Lack of calcium and vitamin D impairs bone formation and strength. Calcium is essential for bone health, and vitamin D facilitates calcium absorption.
- Sedentary Lifestyle: Physical activity stimulates bone formation. A lack of weight-bearing activities, such as walking or lifting weights, can weaken bones.
- Medical Conditions and Medications: Certain conditions like hyperthyroidism, diabetes, rheumatoid arthritis, and medications like glucocorticoids or certain anticonvulsants can accelerate bone loss.
- Genetics and Family History: A family history of osteoporosis or fractures increases the likelihood of developing osteoporosis.
Symptoms of Osteoporosis
Osteoporosis is often called the “silent disease” because it may not present noticeable symptoms until a bone fracture occurs. Common symptoms include:
- Back Pain: Fractures in the vertebrae can cause persistent back pain, which may worsen with time.
- Loss of Height: Compressed or fractured vertebrae can lead to a gradual reduction in height.
- Stooped Posture: Fractures in the spine can cause kyphosis, or a forward-hunched posture.
- Bone Fractures with Minor Trauma: Individuals with osteoporosis may experience fractures with minor falls or even normal daily activities, especially in the spine, wrist, and hip.
Risks Associated with Osteoporosis in the Spine
Osteoporosis refer to increases the risk of fractures, especially in the spine, hip, and wrist. Spinal fractures, or vertebral compression fractures (VCFs), are particularly serious and have several consequences:
- Chronic Pain: Vertebral fractures often cause persistent back pain, which can be severe and long-lasting.
2. Spinal Deformities: Multiple compression fractures can lead to a hunched or stooped posture, impacting balance and mobility.
3. Loss of Height: Vertebral fractures can cause a visible reduction in height, often up to several inches in severe cases.
4. Reduced Quality of Life: The pain and limited mobility associated with spinal fractures reduce an individual’s ability to perform daily activities and impact mental health.
5. Increased Mortality: Studies show that hip and spinal fractures can shorten life expectancy, especially in older adults.
Diagnosis of Osteoporosis
1. Bone Density Test (DEXA): The primary test for diagnosing osteoporosis is dual-energy X-ray absorptiometry (DEXA). This scan measures bone density, usually in the hip and spine, to determine bone loss and fracture risk.
2. X-rays: While not as sensitive as DEXA, X-rays can reveal existing fractures in the spine or other areas. They are often used to identify fractures after a fall or injury.
3. Bone Turnover Markers: Blood or urine tests for markers of bone resorption (e.g., CTX) and bone formation (e.g., P1NP) help assess bone metabolism, which can guide treatment choices.
4. Blood Tests: Blood tests for calcium, vitamin D, and hormone levels can identify underlying causes of osteoporosis or co-existing conditions contributing to bone loss.
5. FRAX Score: The FRAX (Fracture Risk Assessment Tool) helps evaluate fracture risk by considering various factors like age, sex, weight, smoking status, and prior fractures.
Prevention of Osteoporosis
1. Adequate Calcium and Vitamin D Intake: Adults should consume 1,000-1,200 mg of calcium daily and 600-800 IU of vitamin D. This is achievable through diet and supplements if necessary.
2. Weight-Bearing Exercises: Regular weight-bearing activities, such as walking, jogging, and strength training, promote bone formation and maintenance.
3. Avoiding Tobacco and Excessive Alcohol: Smoking and heavy alcohol consumption contribute to bone loss, so avoiding these substances can help prevent osteoporosis.
4. Fall Prevention: Reducing the risk of falls, especially in older adults, is crucial to prevent fractures. Home modifications, using assistive devices, and balance exercises can help reduce fall risk.
5. Bone Density Testing: Early screening with DEXA can detect low bone density and allow for preventive measures before fractures occur.
6. Medication Management: For individuals on medications like steroids or anticonvulsants, regular monitoring and, if possible, alternatives can help reduce osteoporosis risk.
Treatment of Osteoporosis
Lifestyle and Dietary Modifications
1. Nutrition: Ensure adequate calcium and vitamin D intake, either through diet or supplements. Other nutrients like magnesium, vitamin K, and protein are also essential for bone health.
2. Exercise: Weight-bearing and muscle-strengthening exercises strengthen bones and improve balance, reducing the risk of falls and fractures.
3. Smoking Cessation and Limiting Alcohol: Reducing these habits can slow bone loss and improve overall health.
Medications for Osteoporosis
- Bisphosphonates: The most commonly prescribed drugs for osteoporosis, bisphosphonates (e.g., alendronate, risedronate) help prevent bone resorption, reducing the risk of fractures.
- Denosumab: This is an injectable medication that inhibits bone resorption. It is often used when bisphosphonates are ineffective or contraindicated.
- Selective Estrogen Receptor Modulators (SERMs): Medications like raloxifene mimic estrogen’s protective effects on bones, reducing the risk of vertebral fractures.
- Parathyroid Hormone Analogs: Drugs like teriparatide stimulate bone formation and are used in cases of severe osteoporosis.
- Romosozumab: This is a newer medication that increases bone formation and decreases bone resorption, effectively improving bone density.
- Hormone Replacement Therapy (HRT): Used mainly in postmenopausal women, HRT can help maintain bone density. However, it carries certain risks and is often considered for short-term use.
Surgical Treatment in Spinal Osteoporosis
For patients with spinal fractures due to osteoporosis, surgical interventions may be necessary:
1. Vertebroplasty and Kyphoplasty: These minimally invasive procedures involve injecting bone cement into the fractured vertebra to stabilize it. Kyphoplasty also uses a balloon to restore the vertebra’s height before injecting cement. These procedures help relieve pain and restore some stability to the spine.
2. Spinal Instrumentation and Fusion: In severe cases where multiple fractures lead to instability or deformity, surgery with screws and rods to stabilize the spine may be considered. These procedures are complex and often require careful assessment, especially in osteoporotic patients.
3. Robotic-Assisted Surgery: Advanced technologies, such as robotic-assisted systems, can improve surgical precision in spine surgery, particularly beneficial in complex cases with weak bones.
Conclusion
Osteoporosis is a significant health concern that requires early diagnosis, prevention, and treatment to reduce the risk of fractures and associated complications. Lifestyle changes, adequate nutrition, and medication can effectively manage osteoporosis, while surgical interventions can address complex cases, especially in the spine. With early diagnosis and a combination of lifestyle and medical interventions, individuals can maintain bone health and reduce their fracture risk, ensuring a better quality of life as they age.
We’re Here Whenever You Need Us
Phone
+91 85889 64108
Open Hours
BLK Max Hospital ( Mon – Sat : 9AM – 05PM )
Manoyati Clinic ( Tuesday, Thursday, Saturday, Sunday : 5PM – 7PM )
Address
BLK Max Super Specialty Hospital, Rajendra Place, Opd number 4, Ground Floor, Room Number 56, Delhi, 110005